Verify Patient Information
As obvious as it may seem, it often goes unchecked, but verification of patient information is an imperative step in the billing process. Double-check the spelling of patient names, their date of birth, as well as other details that are often easy to overlook or misspell but which can result in filing errors leading to denials of insurance claims later. Have your billing staff go over patient forms that so as to make sure the information received matches with what you process on your claim. This may seem like an insignificant step, but it can expedite the billing process and raise the bar of your profit by omitting the chances of facing denials.
Insurance Cover Verification
Insurance verification is a very important first step when you are trying to keep your orthopedics billing practice continue to profit. Pre-authorizing and verifying coverage provided by the insurance carrier of every patient needs to be performed to make sure they have active coverage for the type of medical services provided to them. It is also imperative to decipher the reports sent to you by the patient’s insurance company. This way you will be assured as to whether or not their policy covers the kind of medical care catered to the patient. Your practice will save time and money by avoiding chances of denials and coverage issues that might have surfaced in the future. Hence, verifying insurance coverage is imperative for a sustainable orthopedic practice.
Timely Filing of Claims
Timely filing of claims can truly benefit streamlining the revenue management cycle of your orthopedic clinic or practice. There needs to be some standard procedures and metrics to make sure that claims are submitted within a stipulated time period. It is also imperative to keep up with the deadlines and filing limitations prescribe by insurance carriers. Meeting the deadlines on time can narrow down the chances of its rejection, ensuring healthy cash flows.
Be Very Code Conscious
It is often the case in orthopedic billing, claims are being denied based on the grounds that the codes used are not specific enough. It is very important that your billing staff are in possession of all the information that is properly documented in order to justify the codes you have selected. It is also incumbent that your staff is using the correct codes for the procedure or services being rendered to the patient. Be aware that ICD-10 requires coding be extremely specific for it to be paid. Your billing staff needs to be properly trained as well as providing them with the necessary resources and expertise for them to be able to document and code the claims to perfection. A good way to discover areas of improvement for your coding staff is Medical auditing. Applying a little attention to codes and coding strategies can vastly increase the revenues of your practice or clinic.
Outsourcing Your Medical Billing
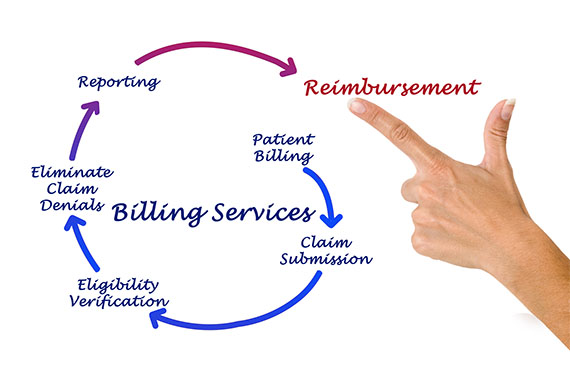
There are many instances where outsourcing the billing management of your orthopedic practice’s billing can vastly decrease the cost of operations of the clinic while increasing the practice or clinic’s revenues. Outsourcing allows your billing process to be more efficient by preventing the delays that result from employee fallouts and turnover, as well as decreasing the overhead expenses and maximize profitability. Outsourcing orthopedic medical billing to specialists who understand the specific coding and billing guidelines for all aspects of orthopedic medical billing, and properly process claims applying specific codes and modifiers is the best way to increase the profits.
Thank you for your interest in RevPro Healthcare Solutions for your Orthopedic Billing Services. Please contact us below or call us at 561-578-8400 with any questions you may have or to request a FREE demo.
Share this article: